CBT (Compatibility mode)
CBT(Compatibility mode)
The carotid body is a small, reddish-brown, oval structure, located in the posteromedial aspect of the carotid artery bifurcation, measures 3-5 mm in diameter and weighs less than 15 mg on average. The gland is highly vascular and receives its blood supply from the external carotid artery. Carotid body tumors (CBTs) are rare neoplasms, constituting approximately 65% of head and neck paragangliomas and develop within the adventitia of the medial aspect of the carotid bifurcation.They originate in the neural crest and are important in the body’s acute adaptation to fluctuating concentrations of oxygen, carbon dioxide and pH.
Carotid body tumors are of three types: Familial (5 -10%), Sporadic (85%) and Hyperplastic (5%). The reported incidence is approx 1-2 per 100,000 population. CBTs are mainly seen in middle age (45-55yrs) but can be seen in younger patients in case of familial type. About 5% of carotid body tumors are bilateral and 5-10% are malignant. The only known risk factors are the presence of chronic hypoxic stimulation and the genetic predisposition. Carotid body tumours can be occasionally coupled with non paragangliomas in syndromes including MEN type II, von Hippel-Lindau syndrome, and neurofibromatosis type 1.
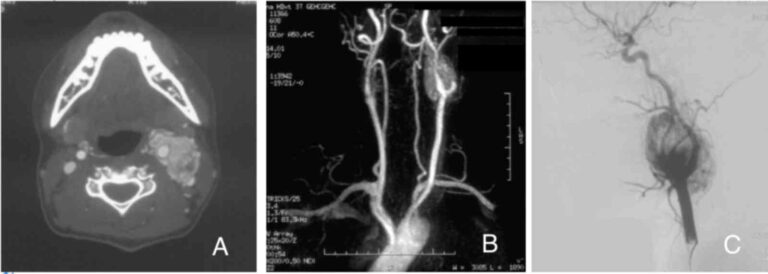
They presents as asymptomatic palpable neck mass in the anterior triangle of the neck, slow-growing tumours remaining asymptomatic for many years, vertically fixed because of its attachment to the bifurcation of the common carotid (Fontaine sign). A bruit can be felt, however, the absence of a bruit does not rule out a carotid body tumor. 10% of the patients may present with pain, hoarseness, dysphagia, Horner syndrome or shoulder drop due to involvement of hypoglossal, glossopharyngeal, recurrent laryngeal or spinal accessory nerve or involvement of the sympathetic chain. When CBTs are functional, symptoms similar to those of pheochromocytoma. such as paroxysmal hypertension, palpitations and diaphoresis, are seen. To rule out functional carotid tumours, urinary catecholamines, vanillylmandelic acid (VMA), and metanephrines should be estimated. Although ultrasonography is good enough for initial diagnosis, CT scan is helpful and typically reveals a hypervascular tumor located at carotid bifurcation. MRI imaging is considered to be the gold standard and shows characteristic salt and pepper appearance on T1-weighted image. MRA provides better insight into the vascularity of the tumour and its feeder vessels.
Accurate diagnosis is usually based on angiographic criteria, which show the typical LYRE sign. Angiography is also helpful in high-risk tumours (Shamblin II or III) that need either embolization or a preoperative balloon occlusion test. Biopsy of carotid body tumors is not indicated. Histologically CBTs are classified into noninvasive, locally invasive, and metastatic types. Unfortunately, malignancy cannot be detected by routine histological findings and is only defined when the tumour metastasizes to regional lymph nodes or more distant sites.
Shamblin described 3 different types or stages of carotid body tumors in 1970. This classification was according to the gross tumor-vessel relationship and was based on the intraoperative findings and postoperative specimen examination. Type I consists of a small tumour that is easily dissected from the adjacent vessels in a periadventitial plane, can be removed without difficulty. Type II tumours are large, more adherent, partially surround the vessel, have moderate arterial attachment and can be removed with care. Type III tumours are larger, completely surround the carotid bifurcation, incarcerate the carotid and nerves and should be approached with great care. Types II and III are more likely to require carotid resection and vascular reconstruction. This classification has been widely used by subsequent authors as a predictor of vascular morbidity and for surgical decision-making. A directly proportional relationship of the Shamblin group with blood loss and surgical time has also been reported
CBT is associated with high rates of morbidity and mortality with mortality rates ranging between 0-3%, stroke 0-8%, and cranial nerve palsy 1-49%. Surgical therapy is the main line of treatment and operative risk is directly related to the size and extent of the tumour. Preoperative embolization is considered in presence of other paragangliomas, bilateral carotid body tumors, age and health of the patient and the patient’s preference, large tumours
Carotid body paraganglioma is a rare neoplasm. Its special anatomical position imposes great difficulty during surgery. Surgical planning and prediction of peri-operative complications can be obtained by digital subtraction angiography, spiral CT angiography and color Doppler imaging. Arteriography, the gold standard for diagnosing CBTs, demonstrates a pathognomonic tumor blush as well as the feeding vessels of the tumor; and is an excellent screening tool for concomitant paragangliomas. Adequate preoperative preparation and embolization of feeding arteries could reduce operative blood loss, improve tumor excision and preserve the internal carotid artery flow
Location
- Maharashtra and Goa
- secretaryvsi@gmail.com
- +1 2123431725
Quick Menus
Newsletters
Be the first to know about exciting new visits,special event and much more
Copyright © 2023 By IMorse Technology Pvt. Ltd.

.png) +
+